Singulair and Mental Health: Neuropsychiatric Concerns Explained
Montelukast's Rise: Benefits Versus Emerging Neuropsychiatric Risks
I began treating young asthma patients when this therapy first became common. It promised fewer attacks and easier nights, a clear clinical win. Stories of regained sleep and lively play were immediate and compelling.
Alongside benefits, reports of mood, insomnia and anxiety started to surface. For some families these effects were subtle; for others, dramatic and distressing. Clinicians began to question whether a link was real or coincidental.
Evidence grew from case reports, observational studies and regulatory reviews, prompting updated warnings. The challenge is balancing symptom control with rare but serious neuropsychiatric signals, a task that requires informed, shared decision making.
Patients and caregivers should be counselled and monitored; report changes in sleep, mood or behaviour promptly. Occassionally stopping treatment may be considered after discussion, but any change should be supervised by a clinician. Stay informed and ask questions early.
| Benefit | Risk |
|---|---|
| Reduced attacks | Sleep/mood changes |
Understanding Reported Symptoms: Insomnia, Anxiety, Mood Swings

Patients often describe nights of restless energy and sudden worry after starting singulair. A mix of sleep loss and heightened arousal can feel alarming; some report abrupt shifts in mood, from irritability to low spirits. These anecdotes sparked more careful monitoring by clinicians and researchers.
Reports have varied in severity and timing; while many experiences are transient, serious events have occured and prompted regulatory reviews. Clinicians advise tracking changes, discussing risks, and weighing benefits of continued therapy and patient preferences. Clear communication helps balance symptom recognition with effective asthma control.
Epidemiology and Evidence: How Strong Are Links?
Large databases and case reports first raised concerns about mood and behaviour changes after singulair use. Observational studies offered mixed signals: some found small increases in depression or self-harm, others reported no clear association.
Randomized trials were not designed to detect rare neuropsychiatric events, so evidence relies heavily on postmarketing surveillance. Meta-analyses attempt to pool data, but heterogeneity and low event rates make firm conclusions difficult and the Occurence of signals variable.
Population studies suggest absolute risk is small, but vulnerable groups like children and those with prior psychiatric history may show higher relative risk. Causality is challenging to establish; temporality and dose relationships are inconsistent.
Shared reporting and research will refine risk estimates. soon.
Mechanisms Proposed: How Montelukast Could Affect Brain

Researchers have proposed several plausible routes by which singulair might influence mood and behavior. Montelukast blocks cysteinyl leukotriene receptors (CysLT1), which modulate inflammation; if the drug crosses the blood–brain barrier, it could shift central immune signalling and microglial activation, subtly altering synaptic pruning and neurotransmitter balance. Animal studies show changes in hippocampal neurochemistry and behaviour, though translation to humans is complex and individual susceptibility may play a big role in why effects have Occured.
Proposed non-inflammatory pathways include altered serotonin and dopamine signalling, disrupted sleep architecture, or effects on neuroplasticity that could manifest as anxiety, insomnia or mood swings. Off‑target interactions, genetic differences in drug metabolism, and concurrent medications may amplify vulnerability. While mechanistic data are intriguing, they remain preliminary; clinicians should weigh biological plausibility against the rarity of events and monitor patients closely, especially children and older adults regularly.
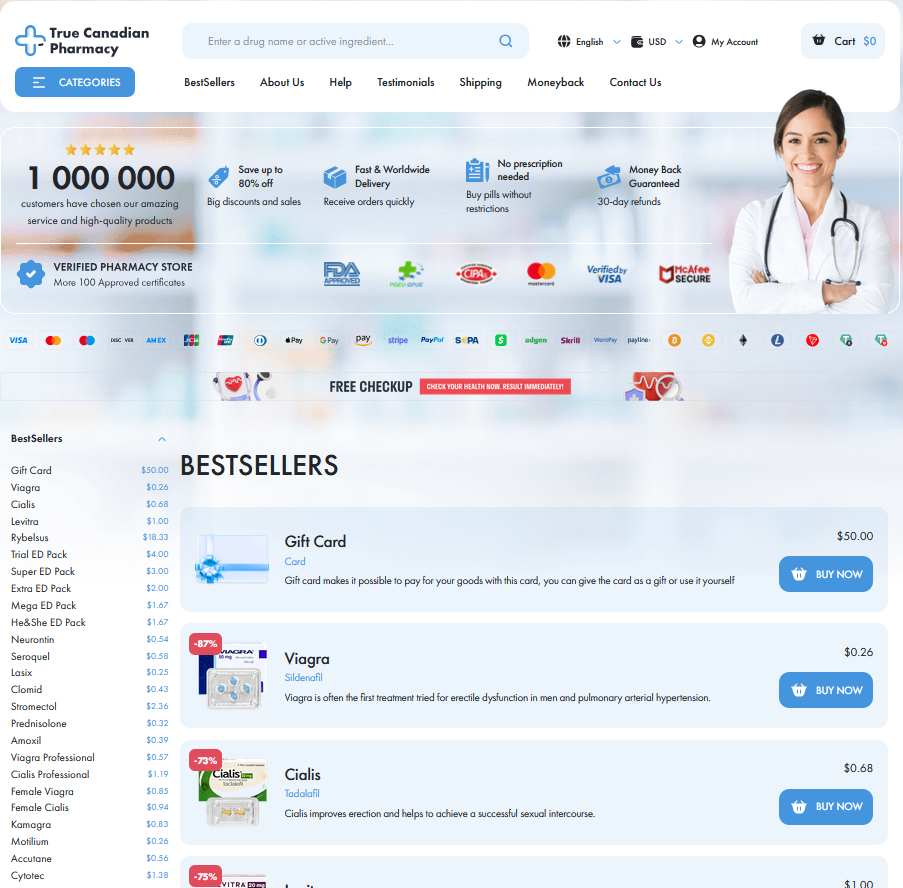
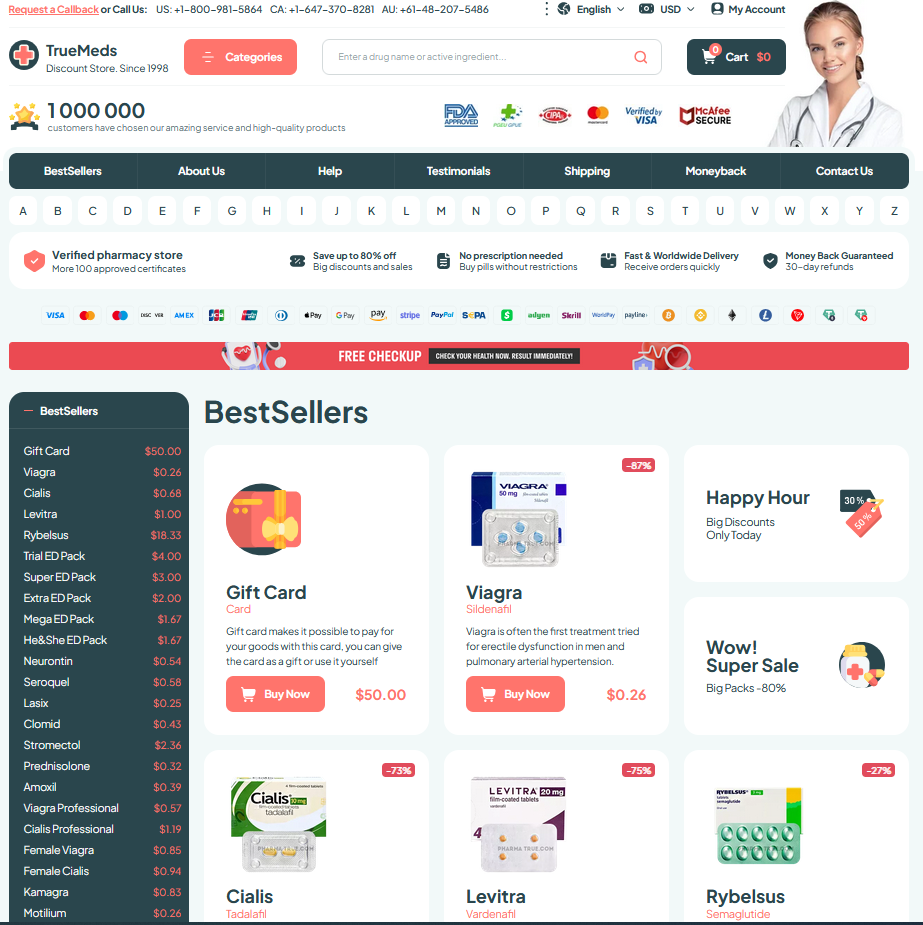
Regulatory Response and Safety Communications Worldwide Explained
Global regulators have shifted from reassurance to caution as reports of mood and sleep disturbances associated with singulair accumulated. Agencies such as the FDA and EMA reviewed clinical trials, postmarketing case series and observational studies, weighing respiratory benefits against possible neuropsychiatric harms. The tone moved from optional advisories to clearer label updates and boxed warnings in some regions, reflecting a growing consensus that prescribers and patients need better informed consent.
Health authorities issued public advisories, clinician guidance, and urged adverse-event reports to pharmacovigilance systems; some nations limited use in children and promoted alternatives. Actions aim to balance safety with continued access while evidence accumulates. Patients must monitor mood and sleep and to Recieve clear counselling; clinicians should report suspect events to improve surveillance and inform future regulatory decisions and update labeling where necessary to protect.
| Agency | Action |
| FDA | Label update |
Practical Guidance: Monitoring, Alternatives, Talking with Clinicians
Begin by tracking symptoms with a simple daily log: note sleep, mood shifts, and any agitation. Share entries openly with your clinician to guide dose decisions early and expectations.
If neuropsychiatric signs appear, definately consider pausing medication only after discussing risks and benefits. Alternative therapies or inhaled corticosteroids may be safer for some patients and explore nonpharmacologic options.
Maintain open follow up: ask about timing of symptoms, suicidal thoughts, or severe mood change. Shared decision making helps balance asthma control with mental wellbeing and patient's goals. FDA EMA