Mebendazole Vs Vermox: What's the Difference?
How Mebendazole and Vermox Work Differently
In clinic I watch tiny parasites meet two different enemies.
Teh one drug locks parasite tubulin to block nutrient uptake, the other disrupts energy use and mobility.
Mechanisms shaped treatment choices.
| Mebendazole | Vermox |
|---|---|
| Inhibits tubulin | Alters glucose uptake |
Clinicians choose based on parasite type, severity, and patient factors. Understanding these distinctions helps patients recieve faster relief and avoids unnecessary repeat treatments. Patients should discuss options with providers to match efficacy with safety and convenience and cost.
Which Parasites Each Drug Effectively Targets

When you picture a parasite lab, familiar names appear: mebendazole and vermox. Both disrupt worm metabolism but favor different targets, so clinicians choose based on the likely culprit and local patterns. This dynamic feels like choosing a scalpel versus a pair of scissors—each best for a job.
Mebendazole often excels against pinworms, roundworms, and certain hookworms; its tissue penetration is limited, making it ideal for intestinal infections. Vermox (mebendazole's common brand) shares much of this coverage but may be preferred in some regions due to availability or dosing. For tapeworms and systemic larval infections other agents are required.
Treatment selection also considers patient age, pregnancy status, resistance trends. Teh clinician may switch drugs if symptoms persist; Occassionally combination therapy or longer regimens are needed when single-dose cures fail. Clear diagnosis and follow-up stool exams help tailor care and improve outcomes.
Recommended Dosages, Treatment Lengths, Practical Tips
Many patients remember the relief vermox brought, but recovery blends biology with sensible steps. Begin by confirming the diagnosis with your clinician, noting age, weight and allergies, then coordinate treatment for close contacts to reduce risk of reinfection; Teh goal is a clear endpoint and a plan for follow-up testing when advised.
Adherence matters: take every dose on schedule, be aware of food or drug interactions, and store medicines as labeled. If symptoms persist, new signs develop, or pregnancy is confirmed, stop treatment and consult a provider quickly. Practical measures such as handwashing, laundering bedding, and avoiding scratching help prevent spread and make pharmacologic therapy far more effective. Children, elderly, and those with liver disease may need tailored monitoring, and discuss vaccination status or community outbreaks with your clinician to align treatment priorities. Keep records of dates and symptoms regularly.
Comparing Side Effects and Safety Considerations

In practice, side effects are often mild and short-lived. Both mebendazole and vermox commonly cause stomach upset, nausea, or transient headaches; more serious reactions like liver enzyme changes or allergic rashes are rare. Patients should stop treatment and seek care if severe symptoms occured.
Safety tips include verifying pregnancy status, avoiding unnecessary repeat courses, and reviewing other medications for interactions. Children require weight-based dosing and monitoring. In prolonged or complicated infections clinicians may request simple blood tests or specialist referral to reduce risk and ensure effective, safe therapy and followup.
Resistance, Treatment Failures, and Clinical Effectiveness
In clinics, clinicians sometimes watch subtle shifts in parasite response when using vermox; patients report persistent symptoms despite therapy. Teh pattern often reflects poor adherence, suboptimal dosing, or true diminished susceptibility. Clinicians should consider confirmatory testing and a tailored second-line plan.
| Issue | Impact |
|---|---|
| Low drug levels | Reduced cure |
| Reinfection | Repeat courses |
Evidence shows single-dose cures work for many species, but efficacy varies by region and parasite burden. When first-line therapy fails, clinicians may repeat dosing, switch agents, or add supportive measures. Surveillance for treatment outcomes and prudent prescribing help limit spread of less responsive strains; patient education on hygiene and adherence remains a high-yield, low-cost strategy to acheive community control and routine follow-up testing post-treatment.
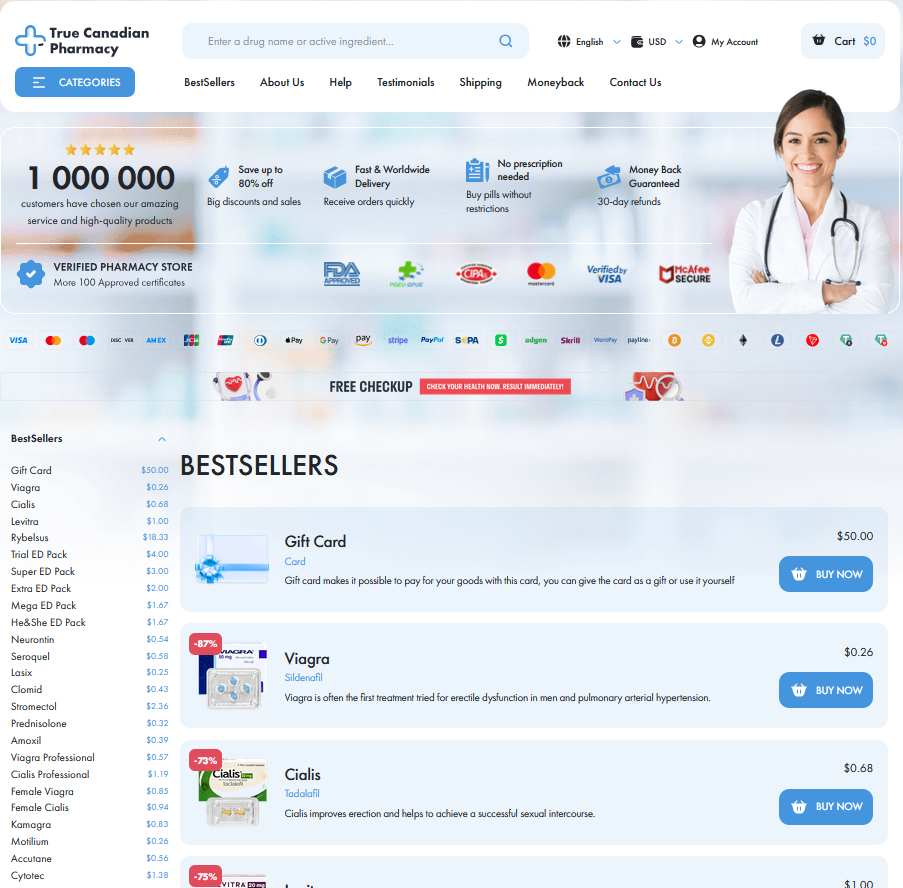
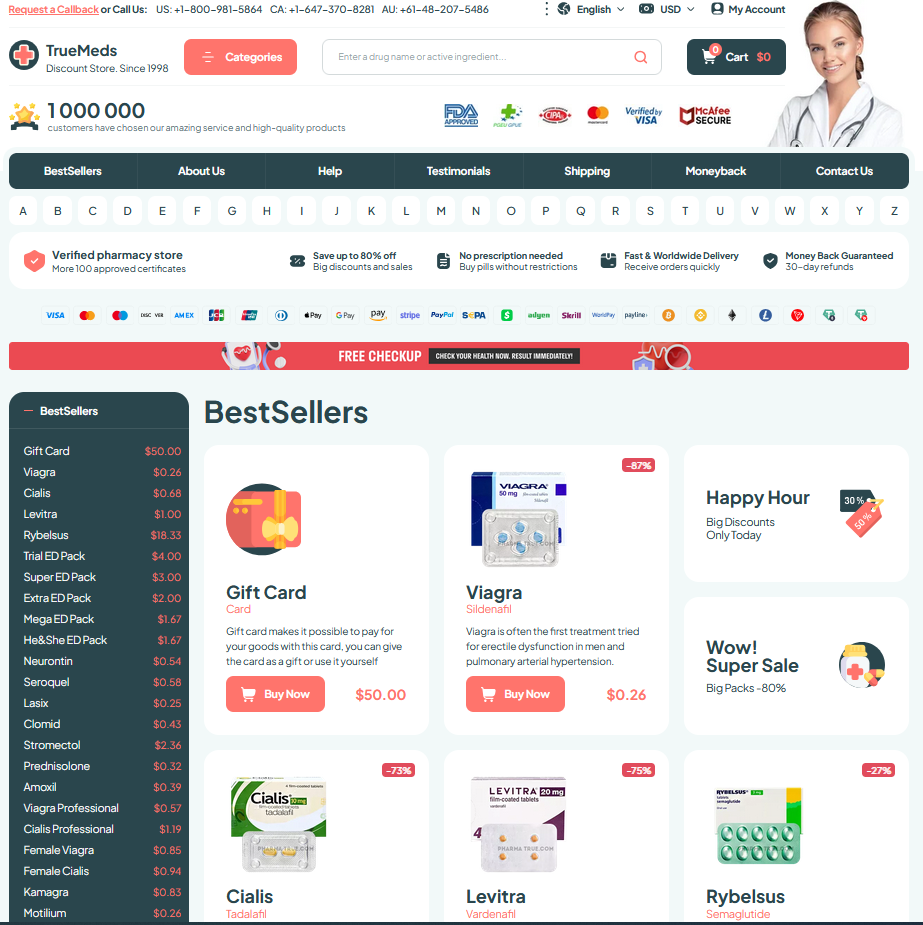
Cost, Accessibility, Brand Names Versus Generics
Many clinicians find generic mebendazole offers identical efficacy to Vermox while being substantially less expensive, so public-health programs can treat more patients without sacrificing quality. Local margins can alter retail pricing.
Availability varies: pharmacies in high-income countries stock both versions, but rural clinics oftentimes rely on generics supplied through essential medicines lists to cover outbreaks, and NGOs fill gaps.
Insurance formularies and procurement policies matter — brand premiums may apply, and travellers should check local licences and import rules if they hope to aquire emergency doses, especially for families.
For many health systems the practical choice balances price, supply-chain stability, and manufacturer reputation; clinicians occassionally prefer brand reassurance, but generics remain clinically sound. Policymakers weigh trade-offs. CDC — Enterobiasis treatment NHS — Mebendazole